CHORIOCARCINOMA
Comprehensive Guide on Symptoms, Causes, Diagnosis, and Treatment

What is choriocarcinoma?
Choriocarcinoma is a rare and aggressive type of cancer that primarily occurs in the uterus or ovaries. It most commonly develops from the tissue that would normally become the placenta during pregnancy, making it a part of gestational trophoblastic disease (GTD). GTD encompasses a group of rare conditions that arise during pregnancy when tumors form from placental tissue, which provides oxygen and nutrients to a fetus.
Choriocarcinoma typically follows a molar pregnancy, where the sperm and egg join incorrectly to form a hydatidiform mole. However, it can also occur after an ectopic pregnancy, miscarriage, or even after a full-term pregnancy. Though predominantly found in women, choriocarcinoma can also affect men as part of a mixed germ cell tumor.
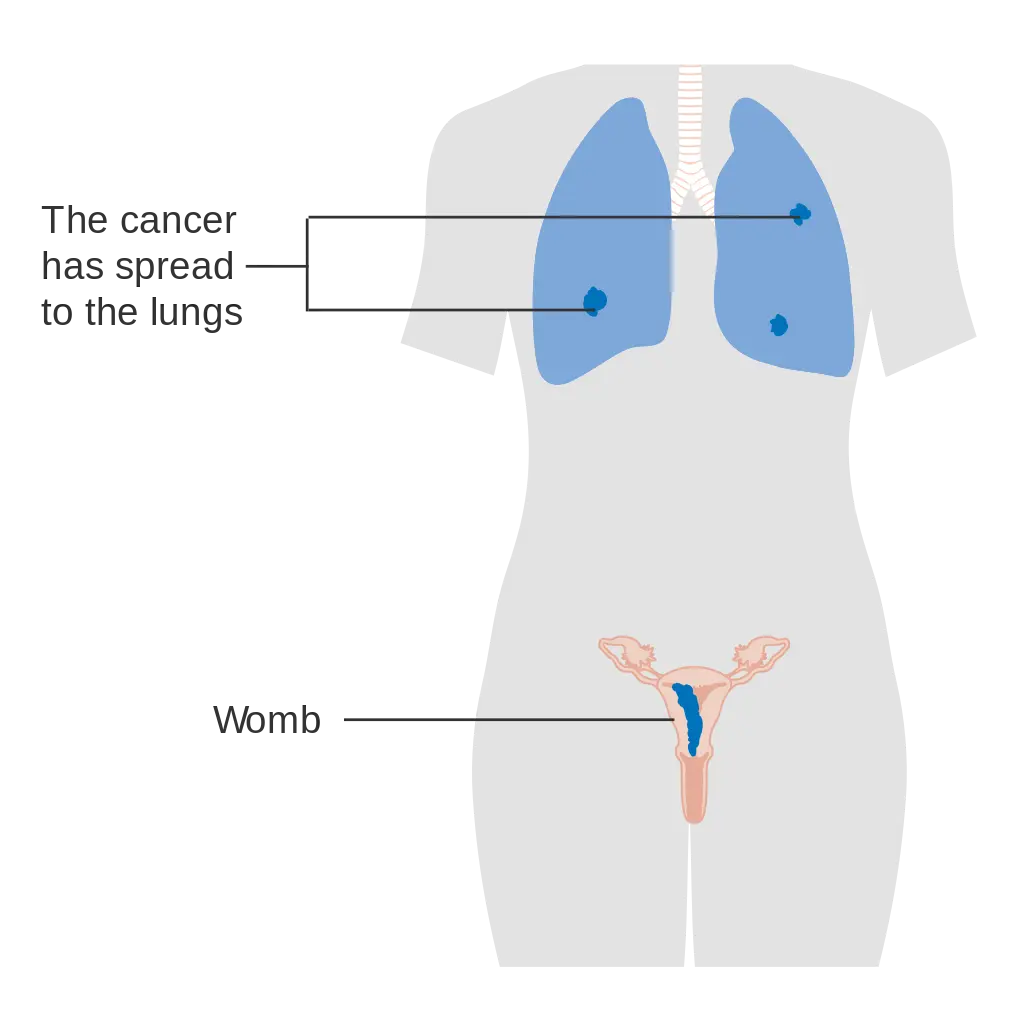
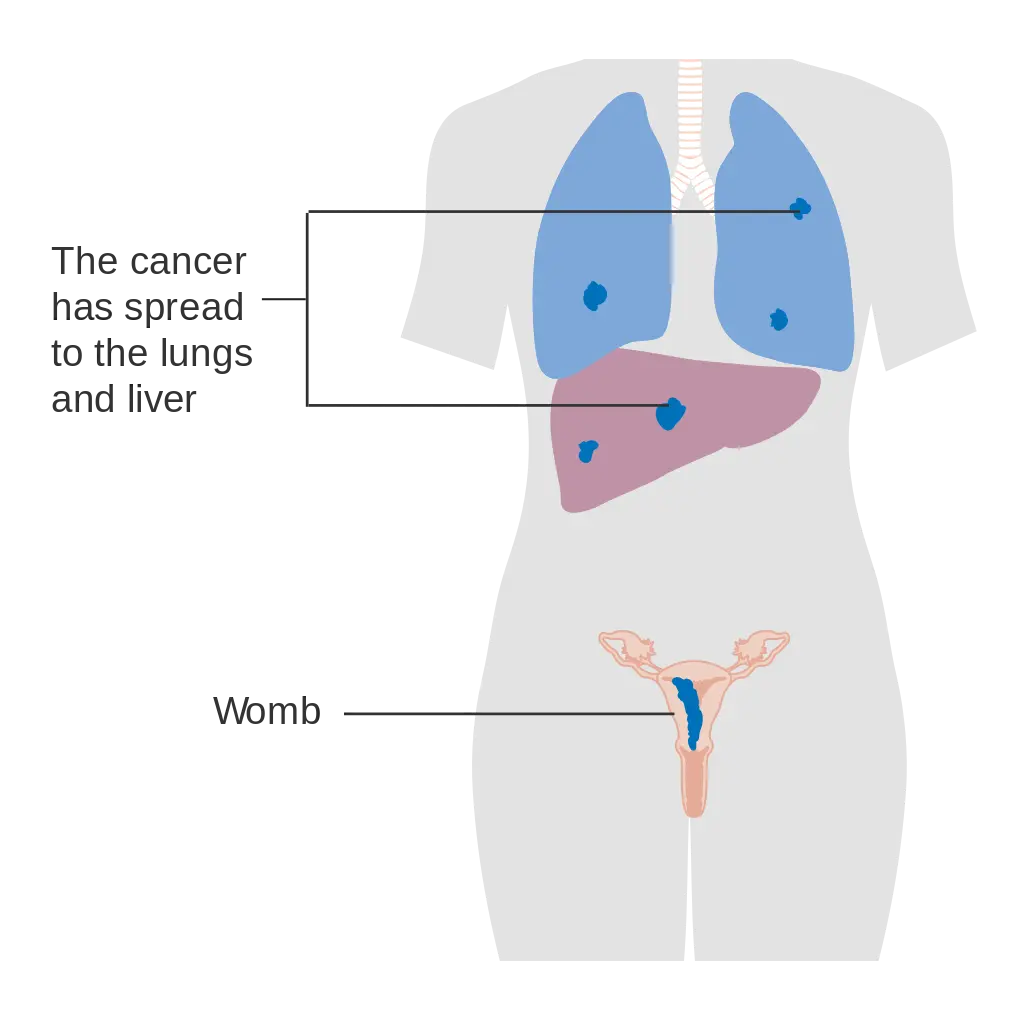
This cancer is known for its rapid growth and ability to spread quickly to other parts of the body, including the lungs, uterine muscle, lymph nodes, liver, kidneys, brain, and blood vessels. Despite its aggressive nature, most cases of choriocarcinoma can be effectively treated with chemotherapy.
In summary, choriocarcinoma is a fast-growing, malignant tumor arising from trophoblastic cells involved in early pregnancy development. While it predominantly affects the uterus, it can metastasize to other organs through the bloodstream, particularly targeting the lungs. With timely medical intervention, including chemotherapy, the prognosis for choriocarcinoma patients is generally positive.
|
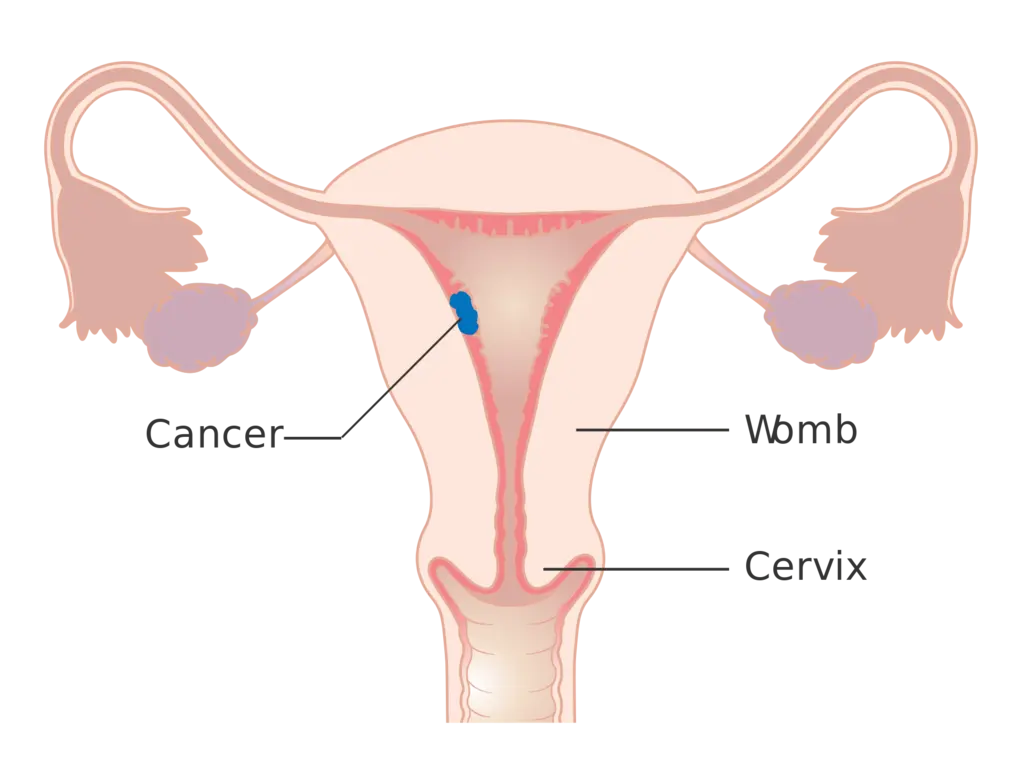
Stage 1 |
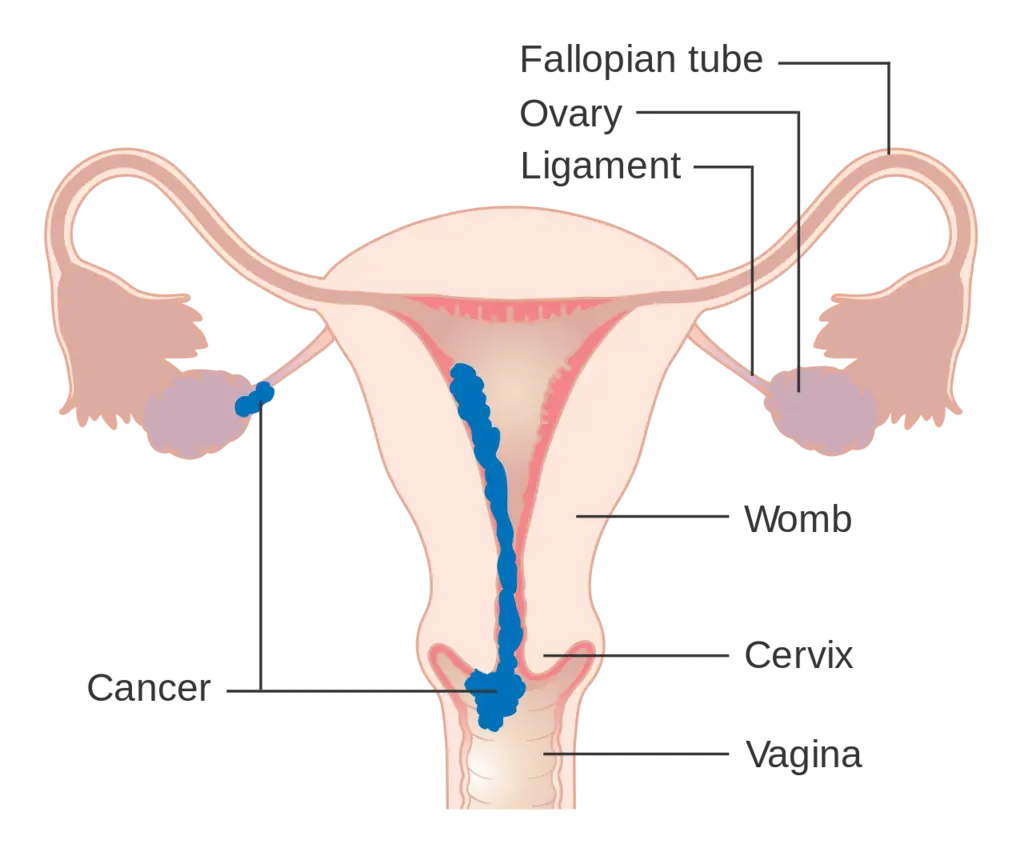
Stage 2 |
Stage 3 |
Stage 4 |
Types of Choriocarcinoma
Choriocarcinoma comes in two types: gestational and non-gestational.
Gestational choriocarcinoma is the more common type. It occurs during pregnancy or shortly after, originating from the placental tissue. This type mainly affects women, developing when something goes wrong with the pregnancy, like in the case of a molar pregnancy.
Non-gestational choriocarcinoma can affect people of any sex. It is a type of germ cell tumor that can develop in the ovaries or the lining of the uterus in women, but it is not related to pregnancy or the placenta. In men, this type can develop in the testicles. Despite being rare, non-gestational choriocarcinoma is significant because it can affect both males and females.
How Common is Choriocarcinoma?
Choriocarcinoma, though serious, is quite rare. Gestational choriocarcinoma makes up about 5% of all cases of gestational trophoblastic disease (GTD). However, GTD itself is uncommon, occurring in about 0.1% of all pregnancies in the United States. To put it in perspective, gestational choriocarcinoma affects fewer than 7 in 100,000 pregnancies in the U.S. This means that while it is more common within the realm of GTD, it is still very uncommon overall. Non-gestational choriocarcinoma, which can affect both women and men, is even rarer.
Choriocarcinoma Symptoms
People with choriocarcinoma, especially those recently pregnant, may experience:
- Irregular vaginal bleeding
- Pelvic pain
If choriocarcinoma spreads to other parts of the body, additional symptoms may include:
- Lungs: Cough, trouble breathing, chest pain
- Vagina: Heavy bleeding, abnormal discharge, lumps
- Brain: Headaches, dizziness, seizures
- Liver or kidneys: Abdominal pain or pressure
Other possible signs are:
- Increased levels of the pregnancy hormone (hCG)
- Shortness of breath
- Coughing up blood
- Testicular cancer in men, sometimes with weight loss, breast enlargement, and skin changes due to hormone imbalances
Choriocarcinoma Causes
These are several of the principal causes of choriocarcinoma
- Choriocarcinoma develops when cells that normally form the placenta during pregnancy, known as trophoblasts, become cancerous. These cells are responsible for supporting the growth of the placenta and fetus.
- About 50% of choriocarcinoma cases are associated with molar pregnancies. In a molar pregnancy, abnormal sacs or tumors develop in the uterus instead of a normal placenta. Even after attempted removal, the tissue can continue to grow abnormally and become cancerous.
- Non-gestational choriocarcinoma can occur in tissues such as the ovaries, testicles, or uterus. In these cases, cancerous cells begin to produce human chorionic gonadotropin (hCG), a hormone normally produced by the placenta during pregnancy.
- The cancer can develop rapidly, months or even years after a pregnancy. It is known for its aggressive nature and ability to spread quickly to other parts of the body.
- Risk factors for choriocarcinoma include experiencing a molar pregnancy, being younger than 20 or older than 40 during pregnancy, or having complications such as ectopic pregnancy.
- Rarely, choriocarcinoma can originate in primary locations other than the placenta, such as the testicles or ovaries. These cases often occur as part of mixed germ cell tumors and are associated with a poor prognosis due to early metastasis and resistance to treatment.
How quickly does gestational choriocarcinoma develop?
There isn’t a set time for how long it takes to develop. It can occur months or years after a pregnancy. It spreads quickly and is considered an aggressive type of cancer.
What are the risk factors for this condition?
Anyone who’s been pregnant (miscarriage, ectopic, termination or full-term pregnancy) can get choriocarcinoma. But you’re most at risk if you’ve had a molar pregnancy.
Other risk factors include: Being younger than 20 or older than 40 during pregnancy.
Diagnosis and Tests
1. Diagnostic Tests for Choriocarcinoma:
- Pelvic exam or physical exam to check for lumps or masses.
- Blood test to measure hCG (human gonadotropin) levels, which are elevated in people with choriocarcinoma.
- Blood tests to assess liver and kidney function.
- Complete blood count (CBC).
- Pelvic ultrasound.
- Computed tomography (CT) scan.
- Magnetic resonance imaging (MRI).
- Chest X-ray.
- These tests can also determine if the cancer has spread.
2. Additional Information:
- A positive pregnancy test (even if not pregnant) due to high hCG levels.
- Enlarged uterus and ovaries may be detected during a pelvic exam.
- Further blood tests include quantitative serum hCG, complete blood count, kidney function tests, and liver function tests.
- Imaging tests (CT scan, MRI, pelvic ultrasound, chest X-ray) help evaluate the extent of the disease.
- Close monitoring after a hydatidiform mole or at the end of pregnancy can improve early diagnosis and outcomes.
3. Criteria for Starting Chemotherapy in Gestational Trophoblastic Disease (GTD):
- Plateaued or rising hCG after uterine evacuation.
- Heavy vaginal bleeding.
- Gastrointestinal or intraperitoneal bleeding.
- Histologic evidence of choriocarcinoma.
- Evidence of metastases in the brain, liver, or gastrointestinal tract.
- Lung opacities greater than 2 cm.
- Serum hCG greater than 20,000 IU/L 4 weeks after evacuation.
- Elevated hCG greater than 6 months after evacuation, even if decreasing.
4. Tests If Suspected Choriocarcinoma:
- Pelvic exam to check for lumps or unusual changes.
- Hormone (hCG) level assessment (high if GTD suspected).
- Blood and urine tests.
- Examination to assess cancer spread to other body parts.
- Imaging tests (CT, MRI, ultrasound, or X-ray).
Management and Treatment

How is choriocarcinoma treated?
Healthcare providers treat choriocarcinoma differently depending on its stage. Staging is how your provider rates your cancer based on the size of the tumor, and if it’s spread to areas outside of your uterus, among other factors. Your overall health and personal preferences are also considered when deciding on a treatment plan.
The main treatment for choriocarcinoma is chemotherapy. Chemotherapy is a drug that kills cancer cells. Some people may also need surgery to remove their uterus (hysterectomy), radiation or a combination of treatments.
After treatment, your healthcare provider will schedule follow-up exams to make sure the cancer doesn’t return.
Is choriocarcinoma cancer curable?
Yes, choriocarcinoma is curable. Treatment with chemotherapy is usually successful in curing it. The prognosis is better when choriocarcinoma is caught early, before it spreads to other parts of your body.
It’s also harder to cure if:
You’ve had chemotherapy and it was unsuccessful.
You develop the disease after a full-term pregnancy or birth of a child.
HCG levels are higher than 40,000 mIU/ml (milli-international units per milliliter) before treatment. HCG is a hormone the placenta creates during pregnancy.
You’ve had symptoms or were pregnant more than four months before treatment.
Prevention
Can I prevent choriocarcinoma?
No, you can’t prevent choriocarcinoma. If you’ve had a molar pregnancy, talk to your healthcare provider about your risk for choriocarcinoma.
Outlook
How long can you live with choriocarcinoma?
The outlook for choriocarcinoma in its early stages is good. The survival rate for people with low-risk gestational choriocarcinoma is almost 100%. The survival rate for people with high-risk gestational choriocarcinoma is 94%.
Non-gestational choriocarcinoma (not related to a prior abnormal pregnancy/placental tissue) has a worse prognosis and is less chemosensitive, which means chemotherapy may not be as effective in killing the cancer cells.
Can Stage 4 choriocarcinoma be cured?
Stage 4 choriocarcinoma means the cancer has spread to other parts of your body like your brain and liver. Your healthcare providers will discuss your outlook with you, but it’s still possible to go into remission.
Living With
Can I still have a baby if I had choriocarcinoma?
Maybe. Many people are able to still have children after treatment for choriocarcinoma. It depends on your diagnosis. Discuss your desire for children with your healthcare provider so they know how to best treat you.
When should I see my healthcare provider?
You should contact your healthcare provider if you develop unusual vaginal bleeding or pelvic pain, especially if you’ve had a molar pregnancy.
A note from Cleveland Clinic
Choriocarcinoma is a rare but serious type of cancer. Receiving a diagnosis can be stressful. But the outlook for choriocarcinoma is generally very good. Discuss your concerns with your healthcare provider and ask them any questions you have about the disease. They’re there to answer your questions and give you the best possible care.
FAQs
Q.How is choriocarcinoma monitored after treatment?
After treatment for choriocarcinoma, regular follow-up exams are crucial to ensure the cancer does not return. These follow-ups typically include monitoring hCG levels, physical exams, and imaging tests like CT scans and MRIs to check for any signs of recurrence or metastasis.
Q.What are the risk factors for developing choriocarcinoma?
The primary risk factors for choriocarcinoma include having had a molar pregnancy, being younger than 20 or older than 40 during pregnancy, and experiencing pregnancy complications such as an ectopic pregnancy or miscarriage. A history of gestational trophoblastic disease also increases the risk.
Q.Can men develop choriocarcinoma?
Yes, men can develop choriocarcinoma, though it is very rare. In men, this cancer can occur as part of a mixed germ cell tumor, usually in the testicles. It is known for its aggressive nature and poor prognosis due to early metastasis and resistance to treatment.
Q.What are the signs that choriocarcinoma has spread to other parts of the body?
When choriocarcinoma spreads, common symptoms depend on the affected organs. For example, if it spreads to the lungs, symptoms may include coughing, chest pain, and difficulty breathing. If it spreads to the brain, symptoms might include headaches, dizziness, and seizures. Abdominal pain and pressure could indicate spread to the liver or kidneys.
Q.What should I do if I have a history of molar pregnancy?
If you have a history of molar pregnancy, it is important to have regular follow-up appointments with your healthcare provider. These appointments will typically involve monitoring hCG levels and possibly imaging tests to ensure any abnormal tissue does not continue to grow and become cancerous. Early detection and monitoring are key to managing the risk of choriocarcinoma.
© 2025 utrunite.org, Inc. All rights reserved.